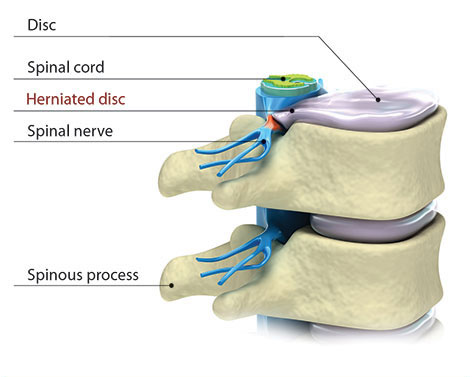
Learn about the shock-absorbing discs that separate the bones in the spine.
Overview | Causes | Symptoms | Diagnosis | Treatment | FAQ
 Spinal stenosis occurs when there is not enough room in the spinal canal for the spinal nerves. Stenosis is a condition that can develop as a person ages, particularly
in those over 50. This condition resembles placing a ring on your finger. If the finger becomes injured or inflamed, the ring constricts and causes pain. The pain caused by stenosis is usually focused in the low back area and can shoot down the legs and can flare up after walking or exercising.
Spinal stenosis occurs when there is not enough room in the spinal canal for the spinal nerves. Stenosis is a condition that can develop as a person ages, particularly
in those over 50. This condition resembles placing a ring on your finger. If the finger becomes injured or inflamed, the ring constricts and causes pain. The pain caused by stenosis is usually focused in the low back area and can shoot down the legs and can flare up after walking or exercising.
Sometimes pain from spinal stenosis can be relieved temporarily by leaning forward or sitting. Pain typically increases when the person bends backward. Stenosis can be treated nonsurgically, but some cases require surgery in order to create more space around the nerves.
Narrowing of the spinal canal may be genetic. However, the primary contributing factor to the development of stenosis is degenerative disc disease. As the spine undergoes changes in stability, density and size, this can result in less space for and more pressure on the spinal structures.
When one area of the spine is injured, it is more likely
that spinal health in other areas will fail. Conditions that may encourage
the development of stenosis include scoliosis, osteoarthritis, rheumatoid
arthritis, spinal tumors and trauma.
[Top]

Symptoms of stenosis include a deep aching in the low back, buttocks
and thigh, and intense numbness or pain in the legs and sometimes
the shoulders. Symptoms can be brought on by walking and exercise.
If you have stenosis, you may notice that pain is sometimes relieved
by sitting or by a position in which the spine is flexed forward
and bending over. Consequently, people with stenosis may walk with
a hunched over posture and find that their pain worsens when bending
backward. Severe cases of stenosis will display more serious symptoms
such as loss of bowel and bladder function and loss of feeling in
an arm/leg.
[Top]
Outlined below are some of the diagnostic tools that your physician may use to gain insight into your condition and determine the best treatment plan for your condition.


In many cases, changing posture and using spinal injections can control the symptoms for a long period of time. Stenosis can be treated nonsurgically, but some cases require surgery in order to create more space around the nerves.
Pain can be relieved by flexing forward and bending over. Taking anti-inflammatories may be beneficial, especially ibuprofen products like Advil or Nuprin. Acetominophen (Tylenol) can be taken for pain, if you are allergic to ibuprofen. A physical therapy program can be followed that incorporates stretches and movements that extend the spine. Injections may be used to reduce inflammation and control pain symptoms. Try our home remedy exercises provided. Stop if they cause an increase in pain or symptoms.
The most common surgery to treat stenosis is called a
laminectomy, which helps create more space for the surrounding spinal
nerves.

For some patients with lumbar stenosis — a narrowing of the spinal canal — walking, standing or arching backward can create pain and numbness in the legs. Traditionally the typical treatment might be a laminectomy to widen the spinal canal to relieve symptoms. In other cases a spinal fusion may be performed to address instability in the spine which is causing similar symptoms.
In 2023 the FDA (Food & Drug Administration) approved a new surgical device that provides an alternative to spinal fusion. While Medicare has decided to cover the cost of the new device as a cost effective alternative to spinal fusion, many other insurance companies often lag behind in covering new technology. So while the TOPS surgery is covered by Medicare, some patients who desire this fusion alternative may have to pay out of pocket — or argue with their insurance carrier to cover the new technology.
Even so, the most advanced spine centers of excellence in the United States, like Mayo Clinic, are being trained in this new TOPS fusion alternative and performing the surgeries for patients who are candidates for the new procedure.
While spinal fusion locks two vertebrae together permanently, the TOPS implant uses a titanium and plastic implant with hinges that preserve the natural motion of the spinal vertebrae. During TOPS surgery, the spine surgeon removes the degenerated and problematic parts of the vertebrae and inserts the TOPS implant.
According to research conducted by the TOPS manufacturer, in a 5 year clinical trial involving 37 spine centers, TOPS had a 85% clinical success rate, compared to spinal fusion which had a 64% success rate. Clinical success included pain reduction, motion preservation and no need for a second surgery.
After surgery TOPS patients reported that they had “less stiffness and greater range of motion, like bending and when trying to put socks and shoes on.
Motion preservation is the holy grail in all types of orthopedic surgery, from knee replacement, hip replacements, shoulder replacements and more recently through artificial disc replacement in the spine that removes a herniated disc but without the need for spinal fusion that locks the vertebrae and can cause herniations later at other levels in the spine.
As with all new technology, insurance companies are often slow to cover new procedures. However, the TOPS manufacturer notes that is changing now as some patients who go through a long appeals process are able to get their insurer to agree to pay for the new surgery. As with any new procedure, there is an unknown about the lifespan of the TOPS implant after 10 to 20 years and revision surgery could be complex.
At Texas Spine and Scoliosis, Dr. Alex Cruz is trained in the TOPS surgery. To learn if you are a candidate, or want to learn more about treatment options for stenosis, complete the appointment request form below.
To learn more about TOPS surgery, click here.
Although degenerating discs are the most common cause of spinal stenosis, spinal tumors, injury, bone disease and other conditions can lead to stenosis as well. For example, primary stenosis results from diseases that are present at birth, while acquired stenosis is typically the result of degeneration in the spine.
If pain interferes with your daily activities, you should consult a spine specialist to treat your stenosis. Leg pain that worsens is especially an indicator of spinal stenosis. This type of pain is not a normal part of the aging process.
Treatment for spinal stenosis aims at minimizing the effects and symptoms of the stenosis but does not stop the progression of degenerative changes. Adopting a healthy lifestyle that includes exercise can help prevent disc degeneration. Click here to learn more about degenerative disc disease.
If your pain is severe enough or if walking has become difficult, your
physician may consider surgery as an option for you. However, nonsurgical,
conservative treatments are usually effective at treating spinal stenosis.
[Top]
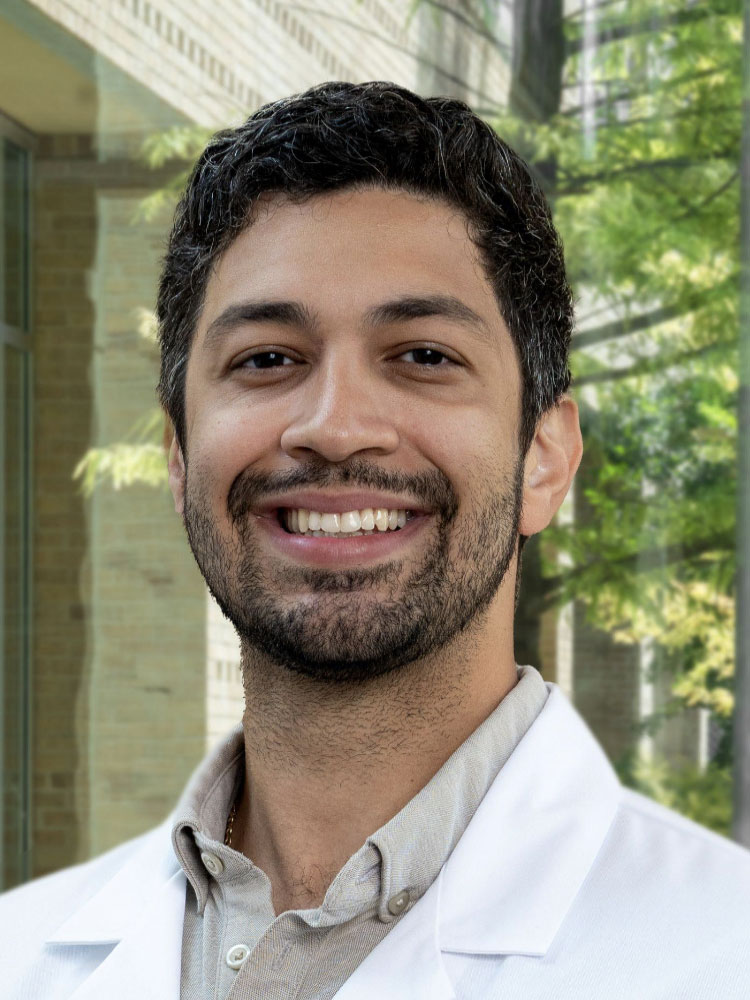
Board-Certified Orthopedic Surgeon
Fellowship-Trained Spine Surgeon
Dr. Alex Cruz is a board-certified orthopedic spine surgeon with sub-specialty training in spine surgery. Dr. Cruz has expertise in minimally invasive and motion preservation procedures of the neck and back, including artificial disc replacement in the neck and low back. Before joining Texas Spine and Scoliosis in Austin in 2024, Dr. Cruz had an active spine surgery practice at Texas Orthopedics in Austin for three years.
Dr. Cruz completed medical school at University of South Florida Morsani College of Medicine, and completed his residency at Baylor College of Medicine in Dallas. He then completed a fellowship in spine surgery at the University of Wisconsin-Madison in 2021. He also completed an AO Trauma Fellowship at the Korea University in Seoul, South Korea in 2019. A fellowship is the highest level of medical education in the United States.