
Learn about nonsurgical options to get you back to your everyday activities.
 Perhaps the most anticipated advance in spine surgery over the past 20 years was the arrival of the artificial disc. The first artificial disc in the United States received formal approval by the Food and Drug Administration (FDA) for widespread use in the United States on October 26, 2004. While this technology is somewhat new to the U.S., artificial discs have been in use in Europe for more than 15 years.
Perhaps the most anticipated advance in spine surgery over the past 20 years was the arrival of the artificial disc. The first artificial disc in the United States received formal approval by the Food and Drug Administration (FDA) for widespread use in the United States on October 26, 2004. While this technology is somewhat new to the U.S., artificial discs have been in use in Europe for more than 15 years.
It is important to remember that this technology is still evolving with new implants continually in development. Your spine surgeon is the best resource to discuss if it is appropriate for you, and what model of artificial disc is best suited for your case.
For example, there are about several models of artificial discs approved by the FDA for use in the United States and the number is expected to grow as new models emerge on the scene and surgeons become trained in their use. Each disc is designed for use either in the low back (lumbar area) or neck (cervical area).
In addition, other artificial disc models are available on a limited basis through “clinical trials” where a patient agrees to be part of clinical study designed to measure the success of a new disc model, which will be part of an FDA study. Patients who participate in a clinical trial can gain access to the most current technology, even though it has yet to gain FDA approval for use in the U.S.
The artificial disc concept is intended to be an alternative for spinal fusion surgery. Each year in the U.S., more than 200,000 spinal fusion surgeries are performed to relieve excruciating pain caused by damaged discs in the low back and neck areas.
During a fusion procedure, the damaged disc is typically replaced with bone from a patient’s hip or from a bone bank. Fusion surgery causes two vertebrae to become locked in place, putting additional stress on discs above and below the fusion site, which restricts movement and can lead to further disc herniation with the discs above and below the degenerated disc. An artificial disc replacement is intended to duplicate the function level of a normal, healthy disc and retain motion in the spine.
When a natural disc herniates or becomes badly degenerated, it loses its shock-absorbing ability, which can narrow the space between vertebrae. In fusion surgery, the damaged disc isn’t repaired but rather is removed and replaced with bone that restores the space between the vertebrae. However, this bone locks the vertebrae into place, which can then damage other discs above and below.
A common aspect of all artificial discs is that they are designed to retain the natural movement in the spine by duplicating the rotational function of a normal healthy disc. Most artificial disc designs have plates that attach to the vertebrae and a rotational component that fits between these fixation plates. These components are typically designed to withstand stress and rotational forces over long periods of time. Still, like any manmade material, they can be affected by wear and tear.
Some of the main benefits of the artificial disc parallel that of knee replacement and hip replacement. This can include the following benefits:

Because of the weight of the body and the rotational stress that the trunk places on discs in the low back (lumbar) area, more stress is placed on artificial discs in the lumbar area than in the neck (cervical) area, which only supports the weight of the head.
A second issue relates to the ease of the artificial disc surgery and any necessary revision surgery to replace a worn out artificial disc. Because the surgeon must access the front of the spine, an incision is made in the abdomen for lumbar discs and in the front of the neck for cervical discs. Generally speaking, many spine surgeons believe access to the cervical discs can be easier than the lumbar discs.
When treating knee and hip replacement patients, orthopedic surgeons try to postpone the implantation of an artificial joint until a patient is at least 50 years old so that they do not outlive their artificial joint, which typically lasts anywhere from 15 to 20 years. Revision surgery, which may be necessary to replace a worn-out artificial joint, can be complex. Unlike knee and hip replacement patients who are typically in their 50s or 60s, many patients can benefit from artificial disc technology at a much younger age — in their 20s or 30s. Therefore, the implantation of an artificial disc in younger patients can raise a surgeon’s concern about the potential life span of the artificial disc in the spine. If the artificial disc wears out, that will require a second revision surgery to replace the worn-out artificial disc. This revision surgery can be far more complex than the initial surgery.
The spine surgeons at Texas Spine and Scoliosis currently use the following artificial discs for the neck:
It is important to understand that not every disc herniation qualifies for an artificial disc. Each patient is evaluated by the spine surgeon to determine if their herniation is appropriate for an artificial disc, and then which artificial disc would be best for each person. For example, some discs come in different sizes to adjust for smaller frames, such as with women and smaller men.
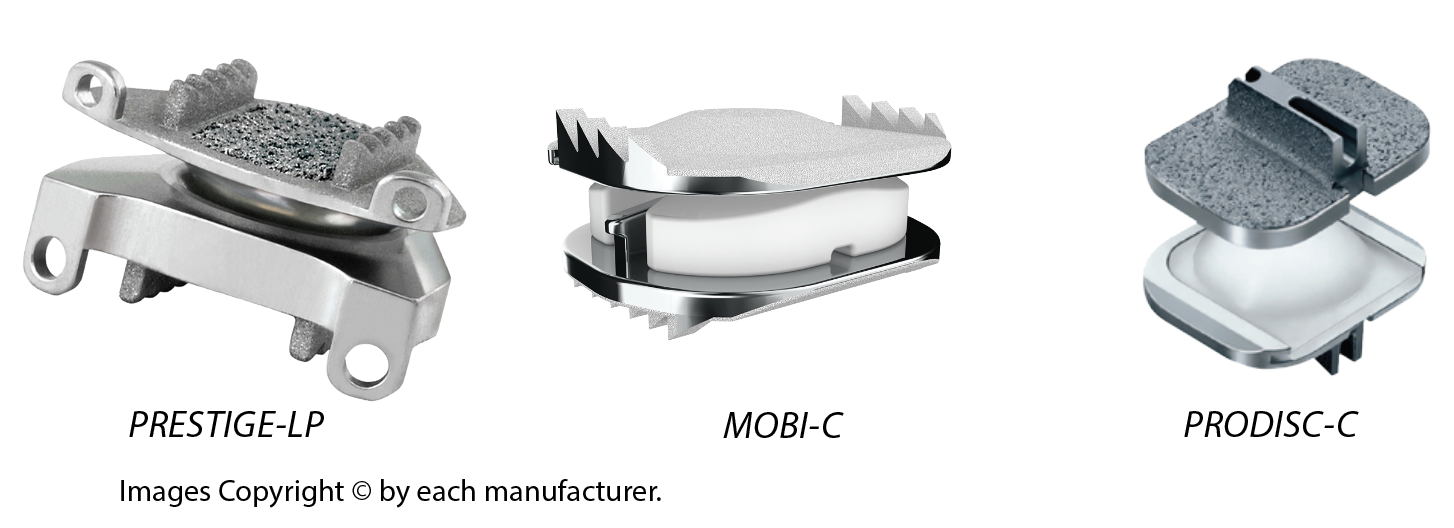
| Feature | Prestige-LP | Mobi-C | ProDisc-C |
|---|---|---|---|
| Material | Titanium-ceramic alloy | Cobalt-chromium + Polyethylene | Cobalt-chromium + Polyethylene |
| Core Type | Ball-in-trough (fixed) | Mobile core | Ball-in-socket (fixed core) |
| Motion Allowed | Good motion, some translation | Full natural motion + translation | Controlled motion, limited translation |
| Fixation | Keel-based | Teeth-based (no keel) | Keel-based |
| FDA Approval | 1-level only | 1-level and 2-level | 1-level only |
| Factor | Best Choice |
|---|---|
| 2-Level Replacement | Mobi-C |
| Most Natural Motion | Mobi-C |
| Maximum Stability | ProDisc-C |
| Durability (Metal-on-Metal) | Prestige-LP |
| Less Bone Removal Needed | Mobi-C |
| Metal Sensitivity Concerns | Prestige-LP |
Most spine surgeons are cautious about artificial disc replacement in the lumbar spine as the technology of lumbar artificial discs is constantly evolving. Unlike the neck which has less weight placed on the artificial disc, the artificial discs in the low back have much more weight on the components which can affect the lifespan of the artificial disc.
Secondly, the front of the neck area is much easier to access than the front of the lumbar spine, as the surgeon must work around internal organs to install the artificial disc. So artificial disc replacement surgery in the low back is more complex.
Thirdly, while the neck has only six disc levels to preserve motion, the back has many more levels to provide rotation, so the option of fusing one level is less problematic to preserving natural rotation.
Lastly, if an artificial disc wears out after 15 to 20 years, revision surgery to remove the old disc and replace it is more complex in the low back than in the neck.
The spine surgeons at Texas Spine and Scoliosis who specialize in artificial disc replacement include: Dr. John Stokes, Dr. Eeric Truumees and Dr. Alex Cruz.
Artificial Disc Surgeons |
||