
Learn more about the providers at Texas Spine and Scoliosis, the only spine specialized neurosurgery, orthopedic surgery, and non-surgical rehabilitation group in the central Texas area.
Osteoporosis occurs when bone resorption (breakdown) outpaces bone formation, leading to reduced bone mass and weakened bone structure. This allows the bones to become porous, fragile, and susceptible to fractures, even from minor stress or falls. Common fracture sites include the spine (vertebral compression fractures), hip, and wrist. Osteoporosis can contribute to conditions like spinal stenosis or herniated discs, which may cause sciatica-like symptoms, and it increases complications in spine surgeries.
 Causes
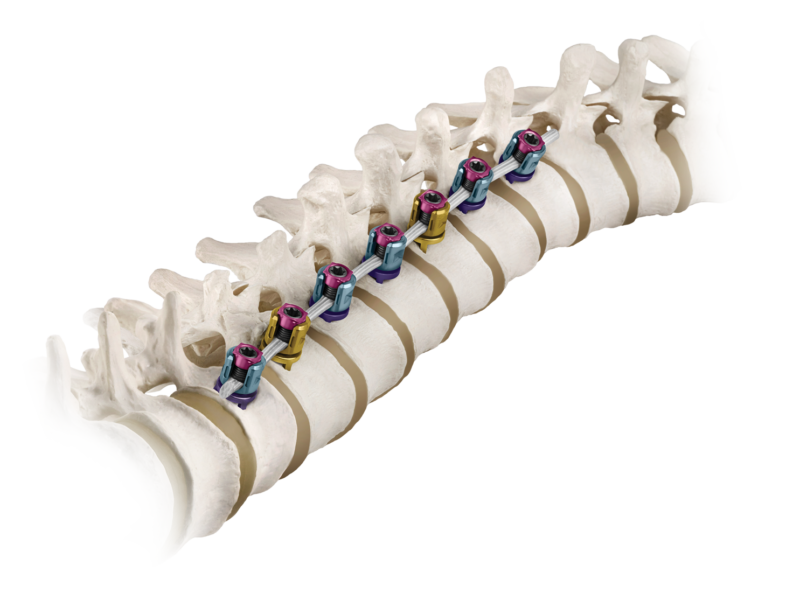
CausesOsteoporosis can significantly increases the risk of complications in spine surgeries, including nonunion (failure of bones to fuse) in procedures that require a fusion. Osteoporotic bones have reduced density and poor bone quality, impairing the ability to form a solid fusion between vertebrae. Nonunion rates in osteoporotic patients can be 20-40% higher than in those with normal bone density, especially in multi-level fusions. Weak bones may not support bone grafts or implants effectively, leading to instability or hardware failure (e.g., screws loosening or breaking).
 Symptoms of Osteoporosis
Symptoms of OsteoporosisOsteoporosis often has no symptoms until a fracture occurs. Common signs include:Bone fractures, especially in the spine, hip, or wrist, often from minor falls or injuries.
Fractures are the most significant symptom, as osteoporosis weakens bones, making them brittle and prone to breaking. Early stages may be asymptomatic, so bone density testing is key for diagnosis.
Osteoporosis is diagnosed through a combination of medical history, physical exams, and specific tests. Here's how:Medical History and Risk Assessment: Doctors evaluate risk factors like age, family history, fractures, smoking, alcohol use, and low body weight.
The DXA scan is the gold standard, typically recommended for women over 65, men over 70, or younger individuals with risk factors.
Managing osteoporosis is critical to reducing spine surgery risks and improving outcomes. Treatment focuses on strengthening bones and preventing fractures:
Texas Spine and Scoliosis is a regional referral center for the treatment of back and neck pain and scoliosis

Learn more about the providers at Texas Spine and Scoliosis, the only spine specialized neurosurgery, orthopedic surgery, and non-surgical rehabilitation group in the central Texas area.
 Texas Spine & Scoliosis approved for the new BRAIVE scoliosis tethering study
Texas Spine & Scoliosis approved for the new BRAIVE scoliosis tethering study

Read about various patient success stories that have been performed by the physicians at Ascension Texas Spine & Scoliosis