
Learn more about the providers at Texas Spine and Scoliosis, the only spine specialized neurosurgery, orthopedic surgery, and non-surgical rehabilitation group in the central Texas area.
In this special Scoliosis Awareness Month segment, we sit down with Dr. Matthew Geck, leading scoliosis specialist, to explore the realities of scoliosis—one of the most common spinal conditions affecting children, teens, and adults. This in-depth interview covers how scoliosis is diagnosed, the latest advancements in both non-surgical and surgical treatment options, and the importance of early detection. Whether you’re a parent, patient, or simply wanting to understand this condition better, this informative discussion sheds light on the signs, symptoms, and solutions available today.
 Do you qualify for an artificial disc?
Do you qualify for an artificial disc?By John Stokes, MD
Board-Certified Neurological Surgeon
Fellowship-trained in Spine Surgery
If you’ve been told that you have a herniated disc in your neck, you may also have been told by the spine surgeon that you need a spinal fusion. The educated patient should explore if that fusion is really the best option long term. Because the standard treatment for herniated discs in the neck has changed over the last five years, and it is also evolving for herniated discs in the low back.
First off, upon further research or with a second opinion, a person may learn that not all herniated discs require surgery. Some can respond to spine therapy or spinal injections to relieve symptoms of radiating pain or numbness in an arm or leg.
However, if non-surgical options fail to relieve the symptoms over a month or so, surgery is typically needed to remove the herniated disc and relieve the pressure on nearby nerve roots. Through a “discectomy” procedure, the damaged disc is removed which then require something is put back into that disc space to keep the vertebrae apart. That can be a bone graft that is inserted between the discs.
This can be the confusing part for a patient with a herniated disc in the neck, because there are many spine surgeons still recommending a spinal fusion for neck herniations. However, this is not always the best recommendation anymore.
Research presented at the North American Spine Society a few years ago documented that spinal fusion in the neck increased the risk of other herniations in the neck. Because the neck has only six disc levels separating the seven vertebrae, locking two levels together reduces the motion in the neck and increases the pressure on the five remaining discs.
A fusion surgery in the neck is called an Anterior Discectomy & Fusion (ACDF), which has been around since 1955. Each year about 150,000 ACDFs are performed. But the number of ACDF surgeries is now decreasing as cervical fusion surgery is replaced by artificial disc surgery in the neck.
The issue is how fast spine surgeons will embrace the most current technology for the patient. It takes significant training and expertise to perform artificial disc replacement, and some surgeons prefer traditional fusion because that is what they are most familiar with — even though there are great patient benefits realized from the motion preservation provided by the artificial disc.
While disc replacement is becoming more commonplace for neck herniations, the same is not yet the case for herniated discs in the low back. There are several reasons for this. One is that the artificial disc technology is still evolving for the low back. While there is less weight placed on the artificial disc in the neck, the discs in the low back have the complete weight of the body and there is more shock absorption needed. The second reason is that accessing the discs in the low back is more complex as surgery involves accessing the disc through the abdomen and around internal organs. Thirdly, there is a concern that the extra weight on the artificial disc in the low back could wear out the disc over 15 to 20 years, which would require replacement surgery which is very complex at a time when the patient is older and has more risk related to any surgery.
With lumbar spine surgery the biggest advance relates to replacing the standard 3-inch incision with a tiny half inch incision where the spine surgeon accesses the disc through a tubular retractor the width of a ball point pen. These patients can go home later the same day, have less blood loss, and less pain in recovery than those who receive a 3-inch incision.
It’s important to remember that the most advanced spine surgery capabilities, both minimally invasive spine surgery through half inch incisions, and artificial disc replacement, are rarely found in small cities. In smaller cities, a person is more likely to find surgeons who split their time between general orthopedics, brain surgery and spine surgery. Not ideal. The ideal is to find a spine specialist who spends 100% of their time on spine surgery, not hips, not knees and not brain surgery. Those are all specialties unto themselves with the same concerns about using the most advanced techniques and instrumention in those niches.
It’s simply not realistic to expect a general orthopedic surgeon or general neurosurgeon to be as proficient with new instruments and artificial discs as a spine surgeon who performs 100 of these surgeries a year. Like anything else, practice makes perfect. The more often a spine surgeon implants an artificial disc the better they get at it and the better the patient’s clinical outcome. Consequently, if you’ve been told you need spine surgery, you will have to travel to a larger city to find a spine surgeon who does a high volume of minimally invasive spine surgery and artificial disc replacement.
Here is some good advice for patients with neck symptoms they suspect are from a herniated disc.
1. For neck herninations, artificial disc replacement can help preserve the natural motion in the neck which can reduce the risk of future herniations.
If you’ve been told you need an ACDF without any consideration for if you qualify for an artificial disc in the neck, you should get a second opinion from another spine surgeon who is proficient in artificial disc replacement. The other reason to do your research on this is because once you have a fusion, it typically can’t be reversed. The issue is that the bone graft can often become fused to the facet joints at the back of the spine. Cutting out and removing the bone graft can then cause a new pain symptom related to the disrupted facet joints. This is why you should determine if you qualify for an artificial disc at the first surgery decision point.
2. Not all neck herniations are appropriate for artificial disc replacement.
While motion preservation is the ideal, not everybody qualifies to have their herniated disc replaced with an artificial implant. If your surgeon is proficient in artificial disc surgery and does not think you are appropriate for it, he probably has determined correctly that you would not have a good outcome from an artificial disc implant.
3. There are many serious neck problems that have similar symptoms but are NOT related to a herniated disc.
Cervical myelopathy and spinal stenosis in the neck may have similar symptoms but relates to compression of the spinal cord rather than a disc herniation. Symptoms can include numbness or pins and needles sensation in the hands, stiffness in the neck or even issues with walking. Cervical myelopathy is a serious condition that if left untreated it can lead to permanent nerve damage including paralysis. Prompt spine surgery is often needed to relieve pressure on the spinal cord.
Spinal stenosis is somewhat common in those over 50 or 60 years of age and relates to bone spurs compressing the spinal cord like a ring on a swollen finger. Spinal stenosis can cause pain as a person arches their back. The good news is that the spine surgery involved is relatively straightforward and outcomes are good.
4. There are other non-disc related issues in the low back.
Lumbar spondylolyssis is a stress fracture of the pars interarticularis in the lumbar vertebrae— a thin bone segment joining two vertebrae. Symptoms of lumbar spondylolyssis includes pain that worsens with running. It can often improve with rest. Lumbar spondylolisthesis is where the cracked vertebra actually slips forward out of position causing instability in the spine. While symptoms can be relieved with rest, surgery may be needed to install instrumentation to stabilize the spine. Lumbar spondylolyssis condition is found in one out of every 20 people but according to the National Institues on health, however, up to 75% of these people may develop spondylolisthesis. Both problems can occur with age, but younger female gymnastics have higher risk. According to National Institutes on Health, spondylolysis and spondylolisthesis affects 10% to 50% of female gymnasts.
5. Be willing to travel to a spine center of excellence for your back or neck.
In summary, if you’ve been diagnosed with a herniated disc in your neck or your back, be willing to travel to a regional spine center that specializes in neck and back surgery, including artificial disc replacement and minimally invasive spine surgery. That way you will be confident that you are receiving the most advanced treatment with the best long term outcome.
Dell Children's Medical Center is the second hospital in the nation activated for use of the new technology
According to the American Academy of Orthopedic Surgeons, scoliosis is a condition that causes the spine to curve sideways. There are several different types of scoliosis that affect children and adolescents. By far, the most common type is "idiopathic," which means the exact cause is not known.
Most cases of idiopathic scoliosis occur between age 10 and the time a child is fully grown. A doctor may recommend surgery if the child's curve is greater than 45 to 50 degrees or if bracing did not stop the curve from reaching this point.
Dell Children’s Medical Center is the second hospital in the nation activated for the Braive™ Growth Modulation System (GMS) investigational study. The study purpose is to determine the safety and probable benefit of the Braive™ GMS when it is used in the treatment of Juvenile or Adolescent Idiopathic Scoliosis.
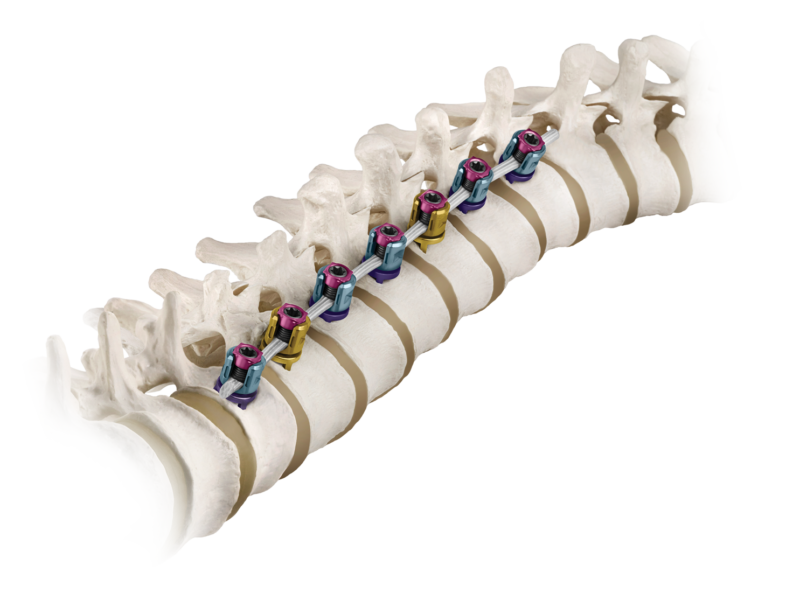
The Braive™ GMS is designed to treat Juvenile or Adolescent Idiopathic Scoliosis. The system features a flexible braid which is attached to the front spinal column using metallic vertebral body screws, plates and set screws. As the patient grows, the braid maintains compressive forces (pushes) on the growth plates of the vertebral bodies along the outward side of the curve to correct the curvature of the thoracic spine. The continued growth of the inward side of the curve brings the vertebral bodies back into alignment. The Braive™ GMS is designed to correct the curve and preserve the patient’s growth potential. For more information about the study and the eligibility criteria, please contact Dr. Matthew Geck, orthopedic surgeon at Ascension Texas Spine & Scoliosis, 512-324-3580.
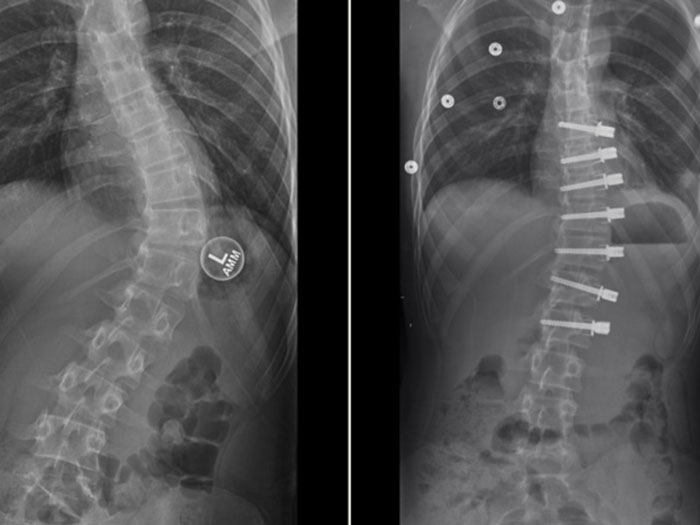
Dr. Matthew Geck, renowned scoliosis surgeon, based in Austin, Texas is the second approved site behind Mayo Clinic to participate in the clinical study assessing the latest BRAIVE vertebral body tether designed by Medtronic.
The Braive study will evaluate the safety and effectiveness in treating adolescent idiopathic scoliosis that is worsening. The Braive system system involves a rope-like braided tether inserted through fixation instrumentation attached to the vertebrae in the spine. Unlike metal instruments that are routinely used in adult scoliosis, the braided tether enables the spine in the adolescent to continue to grow while preventing the curve from worsening.
The hope with vertebral tethering technology in a teenager is that the spinal curve can be arrested while the spine is going through it’s most significant growth period. This may make further scoliosis surgery unnecessary, or less extreme and less risky if it needs to be performed when the patient becomes an adult.
The Medtronic pediatric spine device uses a braid secured to the spine to slow the growth of the curved side of the spine. The clinical study will include patients in the U.S., Canada and the United Kingdom. The first surgery to implant the new BRAIVE technology was done in the United Kingdom at the Newcastle Upon Tyne Hospital.
According to Medtronic, around 4% of children across the globe have scoliosis, which occurs when the vertebrae twist or rotate that may cause the spine to curve into a “C” or “S” shape rather than a straight line. Using a braided tether secured to the spine with screws, the Braive system helps to slow growth on the curved side of the spine while enabling to continue the growth on the other side. The clinical trial will assess whether the system is safe and effective in correcting the spine’s curve in patients with juvenile or adolescent idiopathic scoliosis.
“The goal of the new BRAIVE tether technology is to provide a highly reliable tether that is strong enough to last through adolescence, lessening the risk of the braid fraying or snapping,” according to scoliosis surgeon, Dr. Matthew Geck.
According to the National Scoliosis Foundation, an estimated 30,000 children each year receive a brace in an attempt to arrest the spinal curve. Another 38,000 patients are treated with spinal fusion that locks vertebrae in place. Spinal fusion, however, causes vertebrae to fuse together into a single bone, which stops growth in that area of the spine.
The Braive growth modulation system avoids fusion by using a rope-like braid secured to the spine with screws. This in turn slows the growth on the curved side of the spine, while allowing growth to continue on the other side. The BRAIVE clinical study will evaluate whether the system is safe and effective in correcting the spine's curve in pediatric patients and teenagers with scoliosis.
Within a clinical study, strict criteria is followed related to which pediatric or adolescent scoliosis patients qualify for the last vertebral tether technology.
A subject must meet all of the following INCLUSION CRITERIA to participate in this study:
Additionally the study has specific EXCLUSION CRITERIA, including but not limited to the following:
Patients can contact Dr. Geck’s office related to accessing the clinical study by calling Texas Spine and Scoliosis at 512-324-3580. More information about Dr. Geck is at TexasSpineandScoliosis.com and ScoliosisTexas.com.

Eeric Truumees, M.D., was named president of the North American Spine Society (NASS) during the society’s 35th annual meeting this week.
“I have been a NASS member for 20 years and during that time I have made friends in the spine community around the world and learned a lot about both clinical and non-clinical aspects of spine care,” Dr. Truumees said. “For me, those relationships and the value I have received from my NASS membership, underscore the honor of becoming the NASS president. My predecessors have created an organization that has been modeled by others around the world. I have seen how multidisciplinary organizations like NASS are ideally positioned to represent our patients and our members. For the next year, until our 36th Annual Meeting in Boston in 2021, my goals include broadening our online educational efforts, strengthening our ties to other societies and supporting our outstanding (and ever more important) advocacy work.”
Dr. Truumees is an orthopedic spine surgeon with Texas Spine and Scoliosis, and professor of orthopedic and neurological surgery at the University of Texas, Dell Medical School.
Born in Fort Benning, Ga., Dr. Truumees earned his bachelor of arts degree in biology and religious studies from the University of Virginia and earned his medical degree from UVA as a Bowman Scholar. He completed his residency in orthopedic surgery at the Cleveland Clinic and his fellowship with Harry Herkowitz, M.D., at Beaumont Hospital in Michigan.
Dr. Truumees’ research and academic work has included more than 15 NIH and industry-sponsored multicenter trials, which generated over 30 peer-reviewed publications of original research, 40 invited publications, 50 chapters and monographs and two books. Dr. Truumees has given more than 200 national and international presentations, lectureships and instructorships.
Message from SpineHope Chairman from SpineHope on Vimeo.
There is 1 week left to participate in the WALK TALL Virtual Fundraiser! Help us raise the funds necessary to cover medical and travel costs not being donated to bring Trixia Leongas to Austin, Texas for life-changing spine surgery. There is still time to bid on silent auction items, buy raffle tickets and make donations to sponsor Trixia. To learn more, visit: https://www.32auctions.com/SpineHope2020. Let's together #HealTrixia!
Excerpt from KXAN Austin news story: At the Seton Spine & Scoliosis Center, Dr. Matthew Geck says, “Ten out of 10 doctors would think she needs this. It’s a severe case and it’s not going to do well if we leave it alone.” He is speaking of 15-year-old Suharshi Drbrera, who has been in constant pain for the past four years. She has been wearing a brace to control the pain, but she says it’s made her feel isolated, “I feel uncomfortable when people stare at me, so I just stay home alone all the time.” Read more here.

Leslie was diagnosed with scoliosis as a teenager that was treated first by bracing and then scoliosis surgery with Harrington Rods. Years later she developed Flatback Syndrome.
After two additional surgeries that failed to relieve her condition, Leslie sought a scoliosis surgery revision specialist. She soon learned that in order to find an expert scoliosis surgeon, she must be willing to travel. Leslie traveled out of state to see Dr. Matthew Geck, a Fellowship-Trained Spine and Scoliosis Surgeon. This video details Leslie's journey.
Dr. Geck says scoliosis can cause problems with the lungs and other organs. He says if left untreated, older adults can experience additional symptoms, "...degeneration of the spine, thin bone in older ladies, osteoporosis, and those can cause these curves that have been stable for years to start to progress, so more deformity, more pain."
Read the full article, please click here. Listen to the podcast below.
Update: Watch as Dr. Geck talks with Univision reporter about life saving surgery needed for Arleth. Click here to watch interview.
"We are happy to announce that our first US Hub Program patient is officially on their way to Austin to have surgery at Dell Children's Hospital with SpineHope’s Medical Director & President, Dr. Matthew Geck.
Traveling all the way from Guatemala our 14-year-old patient Arleth and her mother are anxious to finally get the surgical care they've needed for years. Born with a congenital scoliosis, Arleth’s deformity has been the cause of much worry, discomfort and a diminished quality of life.
Though local doctors have been unable to treat her progressive case, it is through SpineHope’s US Hub Program that Arleth will receive appropriate care.
SpineHope is truly indebted for all of the generosity and hard work of all parties involved, which include: American Airlines (their Miles For Kids program), the Austin Ronald McDonald House, Medtronic, Biotronic, Dr. Elena Ruiz (with Bee Caves Pediatrics) and most significantly Dell Children’s Medical Center of Central Texas for making this charity case possible!
Stay tuned for updates on Arleth's visit to Austin and her surgery planned for later this month."
Dr. Matthew Geck and a team of spine specialists on behalf of SpineHope will be traveling to San Jose, Costa Rica on Feb 21st, 2014. The goal of SpineHope is to provide state-of-the-art treatment to children who otherwise may not receive modern treatments for their complex spinal problems.
In order to provide sustainable local care to these children, the SpineHope medical team is equally dedicated to teaching local physicians and staff to provide these treatments themselves. Working together with local physicians, we can correct spinal deformities, remove pain, and often prevent paralysis and extend life.
Watch video above to see how Dr. Geck of Texas Spine and Scoliosis helped Taylor recover from her spinal curve with minimally invasive scoliosis surgery. "It would get serious enough for me to fall to the ground," says Taylor. After minimally invasive scoliosis surgery to correct her spinal curve, Taylor is back on the Varsity Cheer team and recently competed in the Miss Texas Teen USA Pageant. News story feature by JIM BERGAMO / KVUE News and photojournalist Michael Moore.
Click here to read the story on KVUE Austin.
The Becker's listing is comprised of spine surgeons leading scoliosis development nationwide. Dr. Geck is one of only 3 or 4 surgeons in the country to perform truly minimally invasive scoliosis reconstruction, bringing the minimally invasive spine surgery movement to scoliosis surgery in the Southwest United States. These techniques can be used in children, adolescents, and adults. This philosophy is focused on a single, posterior, minimally invasive approach for reconstruction of spinal deformity whenever appropriate. Click here to learn more about Dr. Geck. Click here to view the complete Becker's list of spine surgeons focusing on scoliosis development.
This Becker's Spine Review list is compiled through a lengthy research and review process. The editorial team starts a master list of facilities or individuals based on national rankings or original research. The lists compiled without a nomination process are essentially considered "lists of lists," which highlight institutions or individuals that are consistently lauded by other industry ranking companies.
Each list is vetted through a panel of industry experts. These experts provide feedback on the chosen entries and note any oversights prior to publication.
 Dr. Geck has been using the minimally invasive procedure known as Vertebral Body Stapling for the treatment of spinal curvatures (scoliosis) for the past 2 1/2 years in the Austin region. The treatment is best suited for patients 9-13 years old with spinal curvatures of 25 to 35 degrees. Using a very small incision, a memory medal is placed in the spine which can help straighten the spine while retaining normal motion. The treatment has high success rates, with about 80% of patients seeing either stabilized or improved results after 2 years. Click here to listen to Dr. Geck talk with Perry Watson of KLBJ.
Dr. Geck has been using the minimally invasive procedure known as Vertebral Body Stapling for the treatment of spinal curvatures (scoliosis) for the past 2 1/2 years in the Austin region. The treatment is best suited for patients 9-13 years old with spinal curvatures of 25 to 35 degrees. Using a very small incision, a memory medal is placed in the spine which can help straighten the spine while retaining normal motion. The treatment has high success rates, with about 80% of patients seeing either stabilized or improved results after 2 years. Click here to listen to Dr. Geck talk with Perry Watson of KLBJ.
Dr. Matthew Geck has been selected as a Spine Surgeon Leader to Know by Becker's Spine Review. Click here to visit the Becker's Spine Review site and read more about Dr. Geck.
Becker's Orthopedic & Spine Review features news and analysis on business and legal issues relating to orthopedic and spine practices. Each issue of the quarterly publication reaches an audience of 12,500 key ASC-industry orthopedic and spine practice decision-makers including orthopedic and sports medicine physicians and surgeons and spine practice administrators.
There are four spine surgeons and two nonsurgical care physicians practicing at Texas Spine and Scoliosis. The surgeons perform minimally invasive spine surgery, artificial disc replacement and surgical correction of scoliosis. Click here to read more.
Dr. Matthew Geck is only the third surgeon in central Texas to be accepted into the Cervical Spine Research Society. He was accepted into the society in February of 2012.
The Cervical Spine Research Society is a multidisciplinary organization that provides a forum for the exchange of ideas and promotes clinical and basic science research of the cervical spine. The organization values collegial interaction and strong scientific principles.
Click here to watch the youtube video of Eeric Truumees, M.D. talk about summer back injuries on KXAN.
For many Central Texans, warm weather means an opportunity to become more physically active. But before you grab that golf bag, tennis racket or softball bat, or hit the hike-and-bike trail, an Austin doctor says there are some things you should know to prevent being sidelined with one of the more common injuries. KLBJ's Perry Watson has more in this week's Medical Update.
Click here to listen to Medical Update.

“Vertebral body stapling is a new minimally invasive procedure for patients with early onset scoliosis. The surgeon at Texas Spine and Scoliosis apply metal staples to the front side of the spine between two vertebrae, which compress the growth plates and slow the growth of that side of the spine, allowing the scoliosis to correct themselves naturally, similar to orthodontic braces for teeth,” explains Dr. Matthew Geck, scoliosis surgeon.
READ MORE by downloading the PDF from the Hays Free Press.
Reprinted by permission by Hays Free Press.
 Dr. Matthew Geck shares educational videos and information on spine and scoliosis procedures
Dr. Matthew Geck shares educational videos and information on spine and scoliosis proceduresClick here to watch videos featuring the latest spine surgery and scoliosis surgery techniques and innovations. Videos include Dr. Matthew Geck featured on Austin, Texas news stations. Also view patient educational videos of spine and scoliosis procedures including: "Rod Capture like Sideloading Screws", DLIF procedure, TLIF procedure, XLIF procedure, Scoliosis Care, Patient Success Stories, Minimally Invasive Scoliosis Surgery and more.

A new treatment for scoliosis that is less invasive and risky is helping many patients. Dr. Matthew Geck of Seton and his patient Stephanie Griffin joined FOX 7 to discuss the new minimally invasive scoliosis treatment. Click here to watch (new window will open). Select 'New Treatment for Scoliosis' on the My Fox Austin webpage.

Click here or select the image to the left and learn more about the multidisciplinary spine team at Texas Spine and Scoliosis. The center that combines the expertise of a physical medicine MD, Dr. Lee Moroz, who specializes in non-surgical treatment options and two fellowship-trained spine surgeons, Dr. John Stoke and Dr. Matthew Geck. Listen also as patients of Texas Spine and Scoliosis share their experiences.

Click here or select the image to the left to view a story featuring Dr. John Stokes at Texas Spine and Scoliosis. This story was featured on Austin News KXAN on February 15, 2010.

Click here or select the image to the left to view a story featuring Dr. Matthew Geck at Texas Spine and Scoliosis. This story was featured on Austin News KXAN on February 7, 2010.
 Columbian kids stand tall, thanks to surgeon
Columbian kids stand tall, thanks to surgeonClick here or select the image to the left to view a story featuring Dr. Matt Geck at Texas Spine and Scoliosis.
An Austin doctor says a medical condition that often begins during the teenage years could spell big problems for adults, especially if left untreated. KLBJ's Perry Watson tells us more about this disease in a Medical Update. Click here to listen to this medical update story.
This media clip used courtesy of Radio Station, 590KLBJ, in Austin,Texas.
Geck, Matthew J. MD; Rinella, Anthony MD; Hawthorne, Dana PA; Macagno, Angel MD; Koester, Linda BS; Sides, Brenda MA; Bridwell, Keith MD; Lenke, Lawrence MD; Shufflebarger, Harry MD
Objective. Compare patients with Lenke 5C scoliosis surgically treated with anterior spinal fusion with dual rod instrumentation and anterior column support with patients surgically treated with posterior release and pedicle screw instrumentation.
Summary of Background Data. Treatment of single, structural, lumbar, and thoracolumbar curves in patients with AIS has been the subject of some debate. Advocates of the anterior approach assert that their technique spares posterior musculature and may save distal fusion levels, and that with dual rods and anterior column support the issues with nonunion and kyphosis have been obviated. Advocates of the posterior approach assert that with the change to posterior pedicle screw based instrumentation that correction and levels are equivalent, and the posterior approach avoids the issues with nonunion and kyphosis. This report directly compares the results of posterior versus anterior instrumented fusions in the operative treatment of adolescent idiopathic Lenke 5C curves.
Methods. We analyzed 62 patients with Lenke 5C based on radiographic and clinical data at 2 institutions: 31 patients treated with posterior, pedicle-screw instrumented fusions at 1 institution (group PSF); and 31 patients with anterior, dual-rod instrumented fusions at another institution (group ASF). Multiple clinical and radiographic parameters were evaluated and compared.
Results. The mean age, preoperative major curve magnitude, and preoperative lowest instrumented vertebral (LIV) tilt were similar in both groups (age: PSF = 15.5 years, ASF = 15.6 years; curve size: PSF = 50.3° ± 7.0°, ASF = 49.0° ± 6.6°; LIV tilt: PSF = 27.5° ± 6.5°, ASF = 27.8° ± 6.2°). After surgery, the major curve corrected to an average of 6.3° ± 3.2° (87.6% ± 5.8%) in the PSF group, compared with 12.1° ± 7.4° (75.7% ± 14.8%) in the ASF group (P < 0.01). At final follow-up, the major curve measured 8.0° ± 3.0° (84.2% ± 5.8% correction) in the PSF group, compared with 15.9° ± 9.0° (66.6% ± 17.9%) in the ASF group (P = 0.01). This represented a loss of correction of 1.7° ± 1.9° (3.4% ± 3.7%) in the PSF group, and 3.8° ± 4.2° (9.4% ± 10.7%) in the ASF group (P = 0.028). The LIV tilt decreased to 4.1° ± 3.4° after surgery in the PSF group, and 4.5° ± 3.7° in the ASF group. At final follow-up, the LIV tilt was 5.1° ± 3.5° in the PSF group, and 4.5° ± 3.7° in the ASF group. EBL was identical in both groups, and length of hospital stay was significantly (P < 0.01) shorter in the PSF group (4.8 vs. 6.1 days). There were no complications in either group which extended hospital stay or required an unplanned second surgery.
Conclusion. At a minimum of 2-year follow-up, adolescents with Lenke 5C curves demonstrated statistically significantly better curve correction, less loss of correction over time, and shorter hospital stays when treated with a posterior release with pedicle screw instrumented fusion compared with an anterior instrumented fusion with dual rods for similar patient populations.
Click here to learn more
Geck, Matthew J.; Yoo, Stephen; Wang, Jeffrey C.
During a 7-year period, a consecutive retrospective series of 89 trauma patients at a Level One trauma center who had negative standard radiographs with suspected occult cervical injury were administered a cervical magnetic resonance imaging (MRI) scan. The MRI studies were fully able to assess the ligamentous status of the cervical spine in all patients and were the final step in determining the treatment of the spine. Of the total 89 patients, 82 had no ligamentous injury, and 7 had ligamentous injury. Two patients underwent surgery because of the findings on the MRI study. MRI studies of patients with negative standard radiographs but with suspected occult cervical injury are excellent and safe studies for the evaluation of cervical spinal stability because of their ability to detect ligamentous injuries that are not evident on plain radiographs.
Click here to learn more.
Geck, Matthew J. MD; Macagno, Angel MD; Ponte, Alberto MD; Shufflebarger, Harry L. MD
Objective: To examine a consecutive series of surgically treated Scheuermann kyphosis that had a posterior only procedure with segmental pedicle screw fixation and segmental Ponte osteotomies.
Summary of Background Data: The gold standard for surgical treatment of Scheuermann kyphosis (a rigid kyphosis associated with wedged vertebral bodies occurring in late childhood or adolescence) has been combined anterior and posterior approach surgery. Alberto Ponte has advocated a posterior-only procedure with posterior column shortening via segmental osteotomies, but his procedure has not been widely accepted owing to concerns that without anterior column support there would be a risk of correction loss and/or instrumentation failure. With the advent of improved spinal instrumentation and fixation with thoracic pedicle screws, the Ponte procedure may offer an advantage over anterior/posterior reconstruction.
Methods: The study prospectively enrolled 17 consecutive patients with Scheuermann kyphosis who were treated with the Ponte procedure by the senior surgeon at one institution. Standardized radiographic analysis was performed and included full-length coronal and sagittal radiographs preoperatively, postoperatively, and at final follow-up. Analysis also included the correction obtained through the most severe, wedged segments of the deformity by the osteotomies.
Results: Seventeen patients had the Ponte procedure satisfactorily performed. No patient needed an anterior approach to achieve sufficient correction or fusion. There were no reoperations for nonunion or instrumentation failure. Correction of the instrumented levels was 61% and of worst Cobb was mean 49%. The apex of the deformity was measured over the most deformed 3 to 7 wedged segments. The average correction across the apex was 9.3 degrees per osteotomy (range 5.9 to 15). No patient lost more than 4 degrees of correction through their instrumented and fused levels. There were no neurologic complications. There was one late infection with a solid fusion treated with instrumentation removal and intravenous antibiotics.
Conclusions: Using thoracic pedicle screw instrumentation as the primary anchor, the Ponte procedure was successfully performed in 17 consecutive patients for Scheuermann kyphosis with no exclusions for the size or rigidity of the kyphosis. Results were as good as anterior/posterior historical controls with excellent correction and minimal loss of correction at final follow-up. This procedure avoids the morbidity and extended operative time attributed to the anterior approach.
Level of Evidence: Therapeutic study, level IV [case series (no, or historical, control group)].
Click here to learn more.
https://www.srs.org/professionals/outreach/mission_report_cali-1.pdf
Matthew J Geck, Frank J Eismont
Orthopedic Clinics of North America
April 2002 (Vol. 33, Issue 2, Pages 329-348)
https://www.orthopedic.theclinics.com/issues/contents?issue_key=S0030-5898%2800%29X0001-6
Texas Spine and Scoliosis is a regional referral center for the treatment of back and neck pain and scoliosis

Learn more about the providers at Texas Spine and Scoliosis, the only spine specialized neurosurgery, orthopedic surgery, and non-surgical rehabilitation group in the central Texas area.
 Texas Spine & Scoliosis approved for the new BRAIVE scoliosis tethering study
Texas Spine & Scoliosis approved for the new BRAIVE scoliosis tethering study

Read about various patient success stories that have been performed by the physicians at Ascension Texas Spine & Scoliosis